Paroxysmal Nocturnal Hemoglobinuria (PNH)
Acquired chronic hemolytic disease is caused by complement-mediated hemolysis of complement-sensitive red blood cells.
Although children and adolescents are also affected, it is mainly a disease of adults.
The disorder affects both sexes almost equally.
PNH is chronic, although 15% of patients are known to have a spontaneous remission of PNH within 10-20 years after diagnosis.
Etiology
Defect in PNH caused by pluripotent somatic mutation PIG-A gene hematopoietic stem cells located on the X chromosome.
PNH is an acquired hemolytic disease.
Obviously, the acquisition mechanism of PNH is not yet clear. Therefore, the most fundamental cause of PNH is the cause of gene mutation.
Some mutations are spontaneous and have no cause.
Other mutations are caused by exposure to a mutagen such as radiation or certain chemicals.
Pathophysiology
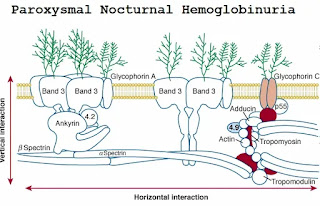
Mutations in the PIG-A gene have blocked the biosynthesis of glycosylphosphatidylinositol (GPI) molecules.
Some proteins attach to the outer cell membrane through GPI anchors.
The physiological purpose of anchoring the unknown-except to anchor itself.
GPI-linked proteins are easily released from the cell membrane.
Proteins that can be transferred between cells.
Blocked GPI biosynthesis leads to a lack of GPI-anchored protein on the surface of hematopoietic cells in PNH patients.
Deficiency of GPI-anchored CD59 (prolectin).
CD59 inhibits the formation of membrane attack complex (MAC) by binding to C8 and C9.
Also, the lack of GPI-anchored CD55 (decay acceleration factor, DAF).
DAF accelerates the degradation of the C3 convertases D4b2a and C3bBb in the classical complement pathway and alternative complement pathway respectively.
Approximately 30 GPI-anchored membrane proteins have been identified in human cells, 20 of which have been proven to be the absence of blood cells in patients with PNH.
In PNH, these GPI-anchored regulatory proteins are either expressed in small amounts or are not present in RBC at all, making them vulnerable to complement-mediated lysis.
Types of mutation differ among patients
- More than 100 PIG-A mutations reported
- All of these will lead to complete lack or severe loss of the function of PIG-A protein.
- Some mutations can cause partial deletion of GPI anchor proteins.
- Most mutations result in non-functional glycosyltransferases and the complete absence of GPI anchor synthesis.
Defects occur in all cell lines derived from mutant bone marrow cells: white blood cells, platelets, and Red blood cells are affected.
Although GPI-anchored proteins can transfer between cells, it does not seem to have a significant transfer to abnormal cells in PNH.
The affected PNH cells are of clonal origin, that is, they appear to be derived from one stem cell.
In some patients, perhaps most patients, there will be 2 or more defective clones.
This could explain the presence of cells with different levels of GPI-anchored proteins
- PNH I cells show normal resistance to lysis
- PNH II cells are 2-5 times more sensitive to complement lysis.
- PNH III cells approximately 25 times more
susceptible to lysis.
Paroxysmal Nocturnal Hemoglobinuria (PNH) phenotypes
Since aberrant cells are more prone to complement lysis, the complete elimination of aberrant clones can be predicted.
In actuality, defective clone dominates over normal cells.
Reasons for this survival advantage not yet known.
The most important hypothesis is the dual pathogenesis idea in which “PNH clones expand relatively in association with the elimination of GPI-positive hematopoietic precursor cells”.
The possibility that CD4+ lymphocytes with CD8+ cytotoxic- T cells take part in the negative selection of PNH clones.
The aberrant clone may have a limited lifespan, which may be due to their spontaneous disappearance and Recover of the patient.
These clones undergo oldness as a result of telomere shortening.
They succumb to autoimmune attack.
Factors promoting their expansion spontaneously remit.
Bone marrow failure
Compared with normal people, the colony formation of erythroid progenitor cells in the peripheral blood or bone marrow of PNH patients and the reduction of granulocyte macrophages and megakaryocyte precursor cells.
Due to proliferation defects rather than complement-mediated progenitor cell lysis, colony formation between GPI-positive and negative progenitor cells in PNH patients is reduced.
Bone marrow failure syndromes contain a plastic anemia (AA), PNH, and myelodysplastic syndrome (MDS).
Hypoplastic or aplastic bone marrow – In PNH, marrow cellularity can range from hypocellular to hypercellular.
Morphological abnormalities in cellular marrow.
Bone marrow failure syndrome is considered a pre-leukemia state.
Up to 10% of patients with PNH develop acute leukemia.
Clinical and laboratory presentations of PNH disappear with the onset of leukemia.
The prognosis of acute leukemia caused by PNH is very poor.
– Functional failure of bone marrow
– Abnormalities in microenvironment and stem cell.
Clinical Presentation
PNH is characterized by paroxysmal intravascular hemolytic attacks.
▪ Brought on by:
- Antecedent infections
- Drug exposure
- Trauma or other stress
- Occurs spontaneously without an identifiable precipitating factor.
▪ Main manifestations:
- Acute hemolysis may manifest as abdominal, lumbar, or sternal pain, or headache, fever, and general malaise.
- Thrombocytopenia can give rise to hemorrhagic
complications in some patients, but thromboses more common.
- Diminished hematopoiesis
- Thrombotic tendency. Especially in abdominal veins
- Hemolytic jaundice
▪ As the disease progresses:
Symptoms due to chronic uncompensated hemolysis:
- Weakness
- Dyspnea
- Pallor
- Iron deficiency
▪ With time, severity relates to the proportion of complement-sensitive cells and the degree of marrow aplasia.
- Budd-Chiari syndrome (hepatic vein thrombosis)
- Intestinal infarction caused by repeated liver and mesenteric vein thrombosis.
- Infections from neutropenia and leukocyte function defects. Exacerbates hemolysis.
▪ With longstanding hemolysis, acute and chronic renal failure may develop
- Enlarged kidneys with excessive iron deposits
- Hematuria
- Tubular malfunction
- Diminished creatinine clearance
- Hyposthenuria
▪ Neurologic complications. Small venous occlusions
▪ Death usually results of:
- Thromboembolism
- Severe exacerbations of hemolysis
- Infection or bleeding associated with aplasia or thrombocytopenia-associated hemorrhage.
Classification of PNH
|
Category
|
Rate of
Intravascular Hemolysis
|
Marrow
|
Flow
Cytometry
|
|
Classic
|
Huge (Macroscopic
hemoglobinuria is frequent or persistent)
|
Cellular morrow with
erythroid hyperplasia and morphology normal or close to normal tomorrow
|
A large population (>
50%)of GPI-AP lacking PMNs
|
|
PNH is associated with
another bone marrow failure syndrome
|
Mild to moderate (Macroscopic
hemoglobinuria is sporadic or absent)
|
Concomitant evidence of bone
marrow failure syndrome
|
Although variable, the
percentage of GPI-AP defective PMN is usually relatively small (<30%)
|
|
Subclinical
|
No clinical or biochemical
evidence of intravascular hemolysis
|
Concomitant evidence of bone
marrow failure syndrome
|
A small population (<
1%)of GPI-AP defective PMNs detected by high-resolution Flow
Cytometry
|
Lab Findings
▪ Urinalysis:
- Nocturnal hematuria/hemoglobinuria
* Classic hallmark of PNH
* Occurs in only about 25-50% of patients
* Begins insidiously
- Infrequent brown urine passed upon awakening
- Hemosiderinuria
- Hemoglobin casts
▪ Iron deficiency – due to hemolysis
▪ Hemolytic anemia (hemoglobin 9-12 g/ml)
▪ Diminished hemoglobin and platelets
▪ Reticulocytosis with macrocytosis
▪ Serum hemoglobin, unconjugated bilirubin elevated
▪ Haptoglobin low or absent
▪ Granulocytes reduced
▪ Bone marrow analysis:
- Erythroid hyperplasia
- Aplasia
- 28% of PNH patients presenting with AA.
▪ Flow cytometry a powerful tool for demonstrating whether cells express or lack specific proteins on surface membranes.
- Gold standard for making the diagnosis
- CD55 and/or CD59 monoclonal antibodies used to diagnose PNH and determine the phenotype of PNH red blood cells
- Regarding sensitivity and specificity, flow cytometry is superior to the old method of complement-mediated hemolysis in vitro
* Ham’s test
* Sugar-water test
* Complement lysis sensitivity (CLS) test
- It was found that more than 1% of CD59 negative cells were considered positive.
- Blood transfusion and extensive hemolysis disturb results.
- Fluorescence-activated cell sorter
(FACS)
* Type of flow cytometry
* Incubate RBC with anti-CD59 mouse monoclonal antibody. After washing, stain with fluorescein-conjugated anti-mouse IgG antibody
* Cells then analyzed using FACS
Sucrose hemolysis test
- Screening test
- The serum pH dropped to around 6.2, and the Mg2+ level was adjusted to 0.005 mol/L to achieve maximum sensitivity.
- Cells that are hemolyzed are the sensitive cells, while cells that remain intact are normal cells, indicating that there are 2-3 RBC subgroups in the circulation
- Test procedure:
* Add one milliliter of patient's citrated whole blood to 9.0 milliliters of fresh sugar water reagent.
* Mix then incubate at room temperature for 30 minutes
* If no hemolysis, then contradicts PNH diagnosis.
Ham or Acidified Serum Lysis test:
- RBCs in PNH are destructed by complement when normal
the serum is acidified or activated by alloantibodies
- Procedure:
* Use patient’s defibrinated whole blood
* Use the patient's RBC to set up the test and control:
– Acidified patient’s serum
– Inactivated patient’s serum
– Patient’s serum
* The test is positive when the patient’s RBCs:
– Hemolyze in their own serum
– Show increased hemolysis in acidified serum
– Do not hemolyze in the inactivated serum
* The control cells showed no hemolysis in all three tubes.
Complement lysis sensitivity test
- More precise
- RBC sensitized with potent anti-I antigen and a limited amount of normal serum as a source of complement for hemolysis.
- This shows 3 groups of RBCs in PNH patients: PNH I cells, PNH II cells, PNH III cells.
Treatment
▪ Treatment of PNH today still mainly symptomatic:
- Blood transfusions are used during periods of severe hemolysis.
- Bone marrow transplantation only available curative therapy
* Risky
* Matching transplants not easily available
▪ Medication
- Anticoagulation therapy indicated during venous thrombotic events
- Immunosuppressive chemotherapy
* When pancytopenia present
* Stimulation of hematopoiesis in aplastic phase
- High doses of corticosteroids considered beneficial
- Androgens stimulate erythropoiesis.
- Complement inhibitor
* Soliris (eculizumab) for treatment of PNH
* The results of the studies showed that treatment with eculizumab can significantly reduce hemolysis and reduce the number of days of hemoglobinuria per month.






Comments
Post a Comment