Neoplastic proliferations of white blood cells - Acute Leukemias (AL)
A. Lymphoid neoplasms, which include non-Hodgkin lymphomas, Hodgkin lymphomas, acute and chronic lymphoid leukemias, and plasma cell dyscrasias and related disorders.
B. Myeloid neoplasms arise from stem cells that normally give rise to the formed elements of the blood: granulocytes, red cells, and platelets.
The myeloid neoplasms fall into three distinct subcategories:
1. Acute myeloid leukemias, in which immature progenitor cells gather in the bone marrow (BM).
2. Chronic myeloproliferative neoplasms in which an inappropriate increase in the production of formed blood components leads to an increase in blood cell counts.
3. Myelodysplastic syndrome is usually related to ineffective hematopoiesis and blood cell reduction.
Acute Leukemias (AL)
There are two major types of AL: acute lymphoblastic (ALL) and acute myeloblastic (AML).
The pathophysiology, laboratory findings, and clinical features of one closely resemble those of the other.
Acute leukemia is usually an aggressive clonal malignant transformation involving the hematopoietic stem cells or early progenitors and characterized by uncontrolled proliferation of blasts in the BM with spillage into the peripheral blood and variable infiltration of other organs.
Etiology of AL
Several factors related to the occurrence of AL include:
I. Environmental Agents
A. Ionizing Radiation
Exposure to atomic bomb explosions is associated with an increased incidence of AL; younger age and those who are closer to the hypocenter are at particularly high risk.
Although ALL has been reported in young individuals, the main type is AML.
Exposure to diagnostic X-rays or radioisotopes at diagnostic levels (low dose) does not increase the risk.
Infants whose mothers were exposed to X-rays during pregnancy are at higher risk.
B. Chemicals
Exposure to the following agents have been noted to be associated with a higher incidence
- Benzene
a. Benzene and other petroleum derivatives
b. Shoemakers and plastic glues
c. Handling buses and trucks
- Alkylating agents: (cytotoxic drugs used to treat certain malignant tumors)
II. Host susceptibility to AL is determined by:
A. Genetic factors
- Fraternal twins and siblings of affected children are at a 2- 4-fold greater risk of leukemia during the first decade of life than are unrelated children.
- If one identical twin is affected, the other twin has a 20% chance of developing ALL.
- Those with Down's syndrome have a 10-30-fold increase risk (> 3y; lymphoid, < 3y; myeloid).
B. Acquired factors; the incidence of AL is increased in related to the following factors:
- Myelodysplastic syndrome
- After chemotherapy + radiotherapy (Secondary AML)
- Chronic myeloproliferative neoplasms (CML, PRV, and MF)
- Aplastic anemia
- Paroxysmal nocturnal hemoglobinuria
III. Oncogenic viruses: there is no good evidence except for HTLV-1, which may cause adult T-cell leukemia/lymphoma.
IV. Others: there is a significant correlation between infants with AL and alcohol intake, smoking, and exposure to benzene and petroleum derivatives of their mothers during pregnancy.
Pathophysiology of Acute Leukemias
- In acute leukemia, differentiation is blocked. This leads to the accumulation of immature leukemic blasts in the BM, which suppress the function of normal hematopoietic stem cells by physical displacement and other poorly understood mechanisms.
- Eventually lead to BM failure, which is the main clinical manifestation of AL.
Acute leukemias have the following clinical characteristics:
- Variable age of onset: ALs can occur at any age, however, childhood AL (age <15 years) is usually ALL (80%) whereas adult AL (age ≥15 years) is usually AML (80%).
- Abrupt stormy onset especially in children
- Symptoms and signs related to BM failure. These include:
• Pallor, weakness, fatigue, lethargy, dyspnea on exertion, angina, and palpitation (due mainly to anemia)
• Fever (reflecting mainly infections resulting from neutropenia)
• Bleeding such as petechiae, ecchymoses, epistaxis, and gum bleeding (secondary to thrombocytopenia).
- Symptoms related to organ or tissue infiltration: Generalized lymphadenopathy, splenomegaly, and hepatomegaly, these are more pronounced in ALL than in AML.
Central nervous system manifestations include headache, vomiting, and nerve palsies resulting from meningeal spread; these features are more common in children than in adults and are more common in ALL than AML. Gum infiltration is more common in AML.
Testicular involvement is more common in ALL. Arthralgia, bone pain, and tenderness.
Laboratory diagnosis of Acute Leukemias
The diagnosis of AL is based on the presence of > 20 % blasts in the BM and/or peripheral blood. However, it can be diagnosed with even < 20 % blasts if specific leukemia-associated cytogenetic or molecular genetic abnormalities are present.
Due to the different responses to treatment, it is of great practical significance to distinguish ALL from AML.
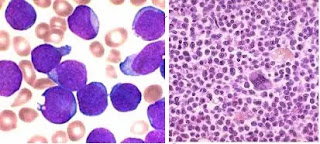
The nuclei of lymphoblasts have somewhat coarse and clumped chromatin and one or two nucleoli; myeloblasts tend to have finer chromatin with multiple nucleoli and more cytoplasm, which may contain granules or Auer rod(s).
• Blood film (BF):
a. RBCs: anemia is usually normochromic normocytic and is almost always present.
b. WBCs: the total WBC count is variable. There may be:
- leukocytosis, where blasts are self-evident, or
- Leukopenia, blasts may or may not be present, or
- it may show a normal count.
Neutropenia is also a common finding in peripheral blood.
c. Platelets: Reduce platelet counts in most cases (ie <150,000/μL or <150×109/L).
• BM aspirate is necessary to confirm the diagnosis (especially when low counts).
• BM trephine biopsy is only essential when:
1. BM aspirate is inadequate; commonly due to BM fibrosis.
2. To distinguish whether a poor aspirate is due to hypocellularity or persistent leukemia.
Investigations
- Hematology: The findings of BF and BM have already been mentioned.
- Biochemical tests may reveal increased S. uric acid, S. LDH, and hypercalcemia. Before starting treatment, take liver and kidney function tests as a benchmark.
- Radiological Examination may reveal
a. Lytic bone lesions.
b. Mediastinal widening caused by an enlargement of the thymus and/or mediastinal lymphadenopathy.
- CSF examination may show blast cell infiltration, indicating CNS involvement.
- If the leukemia is not obvious myeloid cells, cytochemistry is useful.
- Immunophenotyping is indicated in all patients in whom the leukemia is not obviously myeloid.
- Cytogenetic analysis is essential for all patients and is best performed on BM aspiration fluid.
Classification of acute leukemia is based on:
1. Morphology of blasts
2. Cytochemistry using special stains like; SBB, PAS, MPO, Esterases…etc.
3. Immunophenotyping (analysis by flow cytometry and immunohistochemistry).
4. Genetic analysis includes:
- Cytogenetic analysis (applied by conventional karyotyping and FISH techniques)
- Molecular genetic analysis ( by PCR and FISH technology)
Morphological classification
I. French American British (FAB) classification:
A. Acute lymphocytic leukemia (ALL) is divided into three subtypes:
- ALL- L1: Monomorphic blasts, mostly small, high nucleo-cytoplasmic (N/C) ratio, and scanty cytoplasm with small or inconspicuous nucleoli.
- ALL- L2: Heterogeneous blasts, variable sizes, and N/C ratios, prominent nucleoli, irregular nuclear membrane.
- ALL- L3: Monomorphic large blasts with prominent nucleoli and strongly basophilic, vacuolated cytoplasm.
B. Acute myeloid leukemia (AML) is divided into eight subtypes:
- M0: AML, very little evidence of myeloid differentiation
- M1: AML without maturation
- M2: AML with maturation
- M3: Acute promyelocytic leukemia
- M4: Acute myelomonocytic leukemia
- M5: Acute monoblastic M5a/monocytic M5b leukemia
- M6: Acute erythroleukemia
- M7: Acute megakaryoblastic leukemia
II. WHO classification
- There is a consensus that FAB L1, L2, and L3 of ALL are no longer relevant since L1 & L2 morphology does not predict immunophenotype, genetic abnormalities, or clinical behavior.
ALL-L3 is generally equivalent to Burkitt lymphoma in the leukemic phase and should be diagnosed as such.
- The WHO Classification of AML had reduced the blast threshold for diagnosis from 30% (in FAB classification) to 20% in the peripheral blood and/or BM.
Also, patients with certain clonal, recurrent cytogenetic abnormalities should be considered to have AML regardless of the blast percentage.
Cytochemistry of AL
- ALL: is negative for Myeloperoxidase, Sudan Black B, and Non-specific esterases. Periodic Acid Schiff is positive in many cases.
- AML: is positive for Myeloperoxidase, Sudan Black B, and Non-specific esterases. PAS is positive in AML-M6.
Immunophenotyping of AL
This is very useful for typing and subtyping of AL. CD79a is a specific marker for B-cells and CD3 for T-cells. The most specific myeloid marker is anti-myeloperoxidase (MPO).
|
Cell or lineage |
Surface Antigen |
|
Stem |
CD34, HLA-DR, CD45 |
|
B |
CD19, CD20, CD22, CD79a |
|
T |
CD2, CD3, CD5, CD7 |
|
Myeloid |
CD13, CD33, CD117, MPO |
|
Erythroid |
Glycophorin A |
|
Megakaryoblastic |
CD 41, CD61 |
Karyotyping of AL
ALL: the most common karyotypic abnormalities in pre-B-cell ALL is hyperploidy (>50 chromosomes/cell), which is associated with t (12: 21) chromosomal translocation involving the TEL1 and AML1 genes.
The presence of these aberrations correlates with a good prognosis.
Poor outcomes are observed with pre-B-cell ALL that have translocations involving the MLL gene on chromosome 11q23 or the Philadelphia (Ph+) chromosome.
AML: good outcome correlates with t (8:21) & t (15:17) AML: Good results are related to t(8:21) & t(15:17).
Conversely, poor outcome correlates with Ph+, t (6:9), and hyperploidy.
Course & Prognosis of AL
If untreated, patients will only survive for a few months, and they will usually die either of severe infection or bleeding.
Generally, the prognosis of ALL is better than that of AML.T-ALL patients have a better prognosis in adults than in children.
Treatment of childhood ALL (2–10-year age) represents one of the great success stories in oncology and has the best prognosis.






Comments
Post a Comment