Case study (46) – Rifampicin induced thrombocytopenia (ITP)
A 37-year-old woman of African origin is diagnosed as suffering from tuberculosis.
Treatment is commenced with isoniazid (in combination with pyridoxine), rifampicin, and ethambutol.
After 2 weeks of treatment, her legs began to bruise.
Her full blood count shows:
Hemoglobin (Hb) 111 g/L
White blood cells (WBC) 11.7 X 109/L (neutrophils 9.0 X 109/L, lymphocytes 1.8 X 109/L, eosinophils 0.9 X 109/L)
Platelets 6 X 109/L.
A bone marrow aspirate is performed.
Questions:
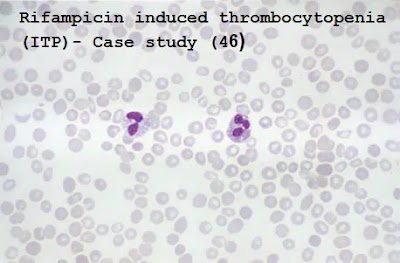
Q1. Comment on the appearance of the blood film and the bone marrow aspirate.
Q2. Why does she have bruising?
Q3. Why is she on pyridoxine?
Answers:
A1. The blood film shows eosinophils, which may indicate drug allergy.
The bone marrow aspirate shows megakaryocytes, and eosinophil precursors are also evident.
A2. She has thrombocytopenia.
The presence of megakaryocytes in the marrow suggests that platelet production is adequate and destruction must be increased.
Immune destruction of platelets is well-recognized as a complication of rifampicin.
Other drugs that can have this effect include heparin, sulphonamides, and thiazide diuretics.
Thrombocytopenia can also occur because of a drug-induced decreased platelet production (e.g. chemotherapeutic and immunosuppressive drugs).
A3. Isoniazid therapy can cause sideroblastic anemia by antagonizing the action of pyridoxine (vitamin B6), thus disturbing heme synthesis.
The image below is an iron stain of bone marrow and shows abnormal iron granules in a perinuclear location (ringed sideroblasts).




Comments
Post a Comment