Case study (48) – Chronic Lymphoproliferative Disorder - Diffuse large B-cell lymphoma
A 75-year-old woman has a history of increasing fatigue for 3 months.
She had generalized lymphadenopathy.
Abdominal examination revealed a palpable
spleen 8 cm below the left costal margin.
Investigations:
- Hemoglobin (Hb) 89 g/L
- White blood cells (WBC) 23.7 × 109/L (lymphocytes 81%, neutrophils 18%)
- Platelets 109 × 109/L
Questions:
Q1. Comment on the blood film.
Q2. Comment on the bone marrow trephine biopsy.
Answers:
A1. The film shows circulating atypical lymphoid cells with cleaved nuclei. The mild thrombocytopenia is due to splenomegaly. The count also shows lymphocytosis.
A2. Biopsy reveals abnormal deposition of mature lymphoid cells along with the trabecular bone-so-called paratrabecular deposition.
Questions:
Q3. What is the differential diagnosis? How would you confirm it?
Q4. The patient developed profound hypothermia and sleepiness 2 years later.
There were no focal neurological signs. A brain computed tomography (CT) scan was conducted.
What complication has occurred?
Answers:
A3. This patient has a chronic lymphoproliferative disorder.
The most likely diagnosis is low-grade follicular lymphoma, confirmed by lymph node biopsy.
Other possibilities would include chronic lymphocytic leukemia and its variants (hairy cell leukemia, splenic lymphoma with villous lymphocytes, prolymphocytic leukemia).
The classification and differential diagnosis of these diseases require careful clinical evaluation, flow cytometry analysis, and cytogenetics.
Molecular profiling can distinguish germinal center B cells (GCB), activated B cells (ABC), and primary mediastinal B cells (PMBL) types.
The ABC types have constitutive NF-κB signaling and features of arrested plasma cell differentiation.
Flow cytometric features of lymphoproliferative disorders:
|
|
CD19/20 |
CD10 |
CD5 |
Other |
|
CLL/Small lymphocytic Lymphoma |
+ |
− |
+ |
|
|
B prolymphocytic leukemia |
+ |
+/− |
−/+ |
MC7+− |
|
Hairy cell leukemia |
+ |
− |
− |
BRAF V600E |
|
Lymphoplasmacytic lymphoma |
+ |
− |
− |
CD11c/CD25c, MY88 |
|
Marginal zone lymphoma |
+ |
− |
− |
BCL−2+ |
|
Follicular lymphoma |
+ |
+/− |
− |
BCL−2+,
t(14;18) |
|
Mantle cell lymphoma |
+ |
− |
+ |
Cyclin D1+ t(11;14) |
|
Diffuse large B-cell lymphoma |
+ |
+/− |
− |
t(14;18), t(3;4) t(2;5) ALK and NPM genes in anaplastic large cell lymphoma |
|
Burkitt lymphoma |
+ |
− |
− |
t(8;14) t(8;22) |
Follicular lymphoma is a germinal Centre cell tumor.
It is histologically categorized into grades depending on the proportion of small cells (centrocytes) to large cells (centroblasts).
Grades 1–2 have a high proportion of small cells and tend to have a low proliferation index (<20%); grade 3 has a higher proportion of large cells and a higher proliferation index (>20%).
The Follicular Lymphoma International Prognostic Index (FLIPI) includes age (>60 versus ≤60 years), stage (III-IV versus I–II), number of involved nodal groups (>4 versus ≤4), anemia (Hb <120 g/L versus ≥120 g/L) and serum lactate dehydrogenase (LDH) (>upper limit of normal [ULN] versus ≤ULN).
The cytogenetic analysis appeared the translocation t(14; 18) is related to the rearrangement of the BCL-2 oncogene and the characteristics of follicular lymphoma.
This translocation leads to an increase in the expression of the anti-apoptotic proto-oncogene BCL-2 by bringing it near to the enhancer sequence of the immunoglobulin heavy chain locus.
Central nervous system (CNS) prophylaxis is considered in those patients with non-Hodgin’s lymphoma (NHL) who are at ‘high risk’ – the major risk factors
being high-grade histology, with a high score on the International Prognostic Index (IPI), involving multiple extranodal sites and testicular involvement, epidural space, paranasal sinuses, and breast.
A4. The CT scan shows a high-density lesion of the hypothalamic region, and this was presumably responsible for her disorder of temperature control and her sleep disorder.
The lesion should not be a biopsy, but her symptoms are responsive to local radiotherapy.
It is likely that the low-grade tumor had transformed into a high-grade neoplasm.
Fungal infections or certain other infection processes may cause similar conditions.
This particular patient also suffered from retroperitoneal lymphadenopathy, which subsequently developed renal failure.
Her central nervous system lymphoma recurred, and she developed visual disturbances.
A repeat CT scan (Figure below) showed a lesion affecting her occipital cortex.
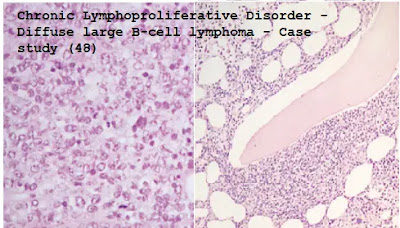
Subsequent lymph node biopsies (Figures below) showed that her histology had progressed from predominantly small cell to large cell (diffuse large B-cell) lymphoma.
Fluorodeoxyglucose positron emission tomography (FDG-PET) scans can show areas of residual disease and help assess response to treatment.
The Figure below shows pre-and post-treatment scans in NHL.
Diffuse large B-cell lymphoma, Fluoroxyglucose-positron emission tomography (FDG-PET) scan. (i) Pre-treatment. (ii) Post-treatment.









Comments
Post a Comment