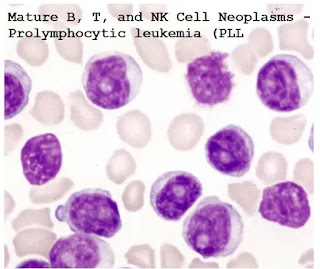
Mature B, T, and NK Cell Neoplasms - Prolymphocytic leukemia (PLL)
In this type of leukemia, the cancer cells are like normal cells named prolymphocytes - immature forms of B lymphocytes (B-PLL) or T lymphocytes (T-PLL).
Both B-PLL and T-PLL are more aggressive than the usual CLL type.
Most people will respond to treatment, but with time they may relapse.
PLL may develop in a patient who already has CLL, but it can also occur in people who have never had CLL.
Phenotypes
1. B-cell Prolymphocytic Leukemia (PLL).
2. T-cell Prolymphocytic Leukemia (PLL).
B-cell Prolymphocytic Leukemia (PLL):
• B-cell lymphocytic leukemia is a very rare disease, mainly defined by the morphological characteristics of circulating monoclonal B cells, lacking both a definite immunophenotype and molecular/genetic characteristics.
• Prolymphocytes, defined as cells with round nuclei, moderately condensed chromatin, and central prominent nucleoli, must exceed a threshold of 55% of lymphocytes, but in practice, most cases exceed 90%.
Epidemiology:
• Incidence:
- Very rare.
- 1% of lymphocytic leukemias.
• Age:
- Usually, > 60 years.
• Gender:
- Male = female.
Clinical Presentation:
- Marked lymphocytosis often with massive splenomegaly.
- Absence of lymphadenopathy.
Prototypic features of B- PLL:
1. CBC:
• The white blood cell (WBC) counts generally exceed 100 x 103/μL (100 x 109/L).
• Anemia and thrombocytopenia in 50%.
• Blood film consists predominantly of prolymphocytes:
Size: A relatively homogeneous population of large cells.
Nucleus: Round nuclei with greatly condensed chromatin and with giant central nucleoli
Cytoplasm: Moderate amounts of pale blue, agranular cytoplasm.
• Prolymphocytes count must exceed 55% but, in most cases, it exceeds 90%.
2. BM examination:
- The leukemic infiltrates are characterized by widely spaced nuclei and prominent central nucleoli.
- Pattern of infiltration:
• It usually shows diffuse or mixed nodular and diffuse nodular patterns of BMB infiltration.
- Reticulin fibrosis may be present.
3. Immunophenotypic analysis:
- Positive B-cell markers: CD20, CD19, CD22, CD79a
- Strongly express surface IgM (+/-)
- FMC7 (+)
- CD5 positive in 1/3 of cases
- CD5(+) CD23(+) cases are more common seen in CLL with PLL transformation.
- CD38 (+) in 57% and ZAP70 (+) in 46%.
•No definitive prognostic value.
•Not related to mutational status of immunoglobulin genes.
- Cyclin-D1 (-)
Differential Diagnosis:
1. CLL/SLL:
- Lower absolute lymphocyte count compared to PLL
- Prolymphocytoid transformation of CLL/SLL shows increased prolymphocytes in peripheral blood and usually is CD23(+) and CD5(+)
- CLL can contain both small lymphocytes and prolymphocytes instead of only prolymphocytes.
- Immunohistochemistry showed that the B cell phenotype has CD5(+), CD23(+), FMC7(-), CD10(-) and weak surface immunoglobulin.
2. Mantle Cell Lymphoma:
- Leukemic variant may have prominent nucleoli and (usually) very high white blood cell counts.
- Misclassified in the past as prolymphocytic leukemia
- CD 5 (+), Cyclin-D1 (+)
- t(11;14) (q13;q32); CCND1/IGH detected by cytogenetic and FISH (Not found in PLL).
3. Splenic Marginal Zone Lymphoma:
- If it is peripheralized, it can show a similar appearance to B-PLL.
- Small lymphocytes, sometimes with abundant cytoplasm.
- May show polar villi.
- B-cell phenotype with CD5(-), CD10(-), and CD23(-).
- Deletion of 7q in ~70%.
4. Hairy Cell Leukemia Variant:
- Condensed chromatin, single distinct nucleolus, and abundant cytoplasm
- Immunohistochemical studies show B-cell phenotype CD11c (+), CD103(+), CD 25(-), CD123(-).
T-cell Prolymphocytic Leukemia (T-PLL):
Synonyms: T-chronic lymphocytic leukemia.
- Despite the controversy, the current recommendation is to combine the diseases formerly known as T-PLL and T-CLL into one disease category.
Due to the similarity of clinical processes and cytogenetic abnormalities, it is best to consider T-CLL as a small cell variant of T-PLL.
Definition:
- Aggressive mature T-cell tumors, characterized by small to medium-sized T cells, usually involve peripheral blood (PB) bone marrow (BM), lymph nodes, and skin.
Clinical issues:
- Incidence: 2% of mature lymphocytic leukemias.
- Age: Elderly; median age: 65 years.
- Sex: Male predominance (M: F = 3:1).
- No environmental, infectious, or ethnic association.
Clinical Presentation
- The white blood cell count is very high: 100 x 109 / L or higher.
- Marked splenomegaly.
- Patients with T-PLL are more common in lymph node enlargement, skin involvement, and pleural effusion.
- Some patients may have a short time before aggressive progression.
- Patients with abnormal ATM genes at 11q22-23 (for example, ataxia-telangiectasia syndrome) have a higher incidence of T-PLL.
Blood findings:
- In some cases, the cells are like those seen in B-PLL, exhibiting round nuclear contours with huge central nucleoli.
- In other cases, leukemia cells show greater nuclear irregularities, often with knobs with cytoplasmic protrusions and blebs.
- In the occasional T-PLL case, nuclear irregularities are close to those seen in SS or ATLL.
The nuclear chromatin is usually condensed, with nucleoli variably prominent but sometimes inconspicuous.
The nuclear chromatin is usually condensed, with nucleoli variably prominent but sometimes inconspicuous. Relatively few cytoplasm is basophilic and granular and may exhibit prominent blebs.
BM examination:
- The BM infiltration of T-PLL has characteristic diffusion and can widely replace hematopoietic cells and adipocytes.
- The nodules and diffuse infiltrates in occasional cases are mixed, and sometimes fibrosis is related to these leukemic infiltrations.
Immunophenotypic analysis:
- Expressed of Pan T-cell markers (CD3, CD2, CD5 and CD7).
- No expression of immature markers such as CD34, TdT, or CD1a.
- CD4(+)/CD8(-) 60%, CD4(+)/CD8(+) coexpression 25-48%,
CD8(+)/CD4(-) 15%.
Cytogenetics:
A consistent cytogenetic abnormality has been identified in 80% of cases of T-PLL.
This abnormality is an inversion (14) (q11q32).






Comments
Post a Comment