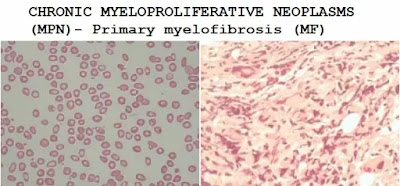
CHRONIC MYELOPROLIFERATIVE NEOPLASMS (MPN)- Primary myelofibrosis (MF)
A clonal disorder of a multipotent hematopoietic progenitor cell of unknown etiology characterized by marrow fibrosis, extramedullary hematopoiesis, and splenomegaly.
Myelofibrosis (MF) is a chronic blood cancer that produces excessive scar tissue in the bone marrow and weakens its ability to produce normal blood cells.
MF is believed to be caused by abnormal blood stem cells in the bone marrow.
Abnormal stem cells produce more mature cells, which grow rapidly and take over the bone marrow, causing fibrosis and chronic inflammation.
As a result, the bone marrow becomes unable to produce normal blood cells, and the production of blood cells may move to the spleen, causing enlargement or transfer to other parts of the body.
MF can be classified as a myeloproliferative tumor (MPN), which can produce spontaneously (primary myelofibrosis, PMF), polycythemia vera (after PV-MF), or essential thrombocytosis (ET- After MF).
The presentations of PMF, PV-MF, and ET-MF are the same, and for these three, the treatment is usually the same.
Pathophysiology:
Myelofibrosis is excessive bone marrow fibrosis and loss of hematopoietic cells, followed by a significant increase in extramedullary hematopoietic function (primarily in the liver and spleen, which enlarge significantly).
The cause is mesenchymal for fetal hematopoiesis reactivated.
Myelofibrosis may be primary or secondary to several hematologic, malignant, and nonmalignant conditions.
PMF is more common than secondary myelofibrosis due to tumor transformation of pluripotent bone marrow stem cells.
Bone marrow fibrosis occurs due to increased secretion of platelets derived growth factor.
These PMF progeny cells stimulate bone marrow fibroblasts (not part of tumor transformation) to secrete too much collagen.
In primary myelofibrosis, a large number of platelets and abnormal megakaryocytes (platelet forming cells) release chemicals that overstimulate fibroblasts.
This leads to the excessive growth of thick and thick fibers in the bone marrow, gradually replacing the normal bone marrow tissue.
Over time, this destroys the normal bone marrow environment, thereby preventing the production of sufficient numbers of red blood cells, white blood cells, and platelets.
This results in anemia, thrombocytopenia, leukopenia, and the production of blood cells in areas outside the bone marrow for example in the spleen and liver, which become enlarged as a result.
PMF peak incidence is between 50 and 70 years of age.
In PMF, large numbers of nucleated RBCs (normoblasts) and granulocytes are released into the circulation (leucoerythroblastic).
Serum LDH level is often elevated. Eventually, bone marrow failure occurs, accompanied by anemia and thrombocytopenia.
Rapidly progressive, chemotherapy-incurable acute leukemia develops in about 10% of patients.
Malignant or acute myelofibrosis is an uncommon variant, and its downhill process is more rapid. This variant is best classified as megakaryocyte leukemia.
In little cases, long time exposure to high concentrations of benzene or high doses of ionizing radiation may increase the risk of primary myelofibrosis.
About one-third of myelofibrosis patients were previously diagnosed with polycythemia (post-polycythemia myelofibrosis) or essential thrombocytosis (post-ET myelofibrosis).
Age and incidence: It is insidious in onset.
The peak incidence of PMF is between 50 and 70 years of age.
Primary myelofibrosis is a rare chronic disease, estimated to be 1 case per 100,000 people.
It can occur at any age but is usually diagnosed as late in life between 60 and 70 years of age.
The cause of primary myelofibrosis remains largely unknown. It can be classified as either a JAK2 mutation-positive (having the JAK2 mutation) or negative (not having the JAK2 mutation).
Conditions associated with myelofibrosis:
1. Malignancies:
- Cancer with bone metastasis
- Hodgkin lymphoma & Non-Hodgkin lymphoma
- Leukemias
- Multiple myeloma
- Polycythemia vera
- Essential thrombocythemia
2. Infections: Osteomyelitis, TB, HIV
4. Hyperparathyroidism
5. Autoimmune disorders: SLE, Systemic sclerosis
7. Gray platelet syndrome
6. Vit D deficiency & Renal osteodystrophy
Clinical Feature:
Age -- 50years and over.
- At the first diagnosis, about 20% of people have no symptoms of primary myelofibrosis, which happens occasionally due to routine blood tests. For others, symptoms develop gradually over time.
- PANCYTOPENIA + ORGANOMEGALLY + CONSTITUTIONAL SYMPTOMS
• Tiredness, weakness or shortness of breath, mild fatigue. These symptoms usually result from anemia or chronic inflammation.
• Because the spleen compresses the stomach and other organs, the upper left part of the abdomen is full, discomfort or pain, and early satiety (accounting for 1/3 of patients).
• About two-thirds of cases also cause abdominal discomfort due to liver enlargement (hepatomegaly).
• Feeling pain or fullness below the ribs on the left side.
• Feeling full sooner than normal when eating.
• Fever, caused by inflammation or infection
• Night sweats caused by inflammation.
• Weight loss or malnutrition due to inflammation and spleen and stomach
• Bone pain
• Itching (pruritus) caused by chronic inflammation
• Low platelet count or impaired coagulation function, easy to bleed or bruise
• Susceptibility to infection due to low white blood cell count or decreased antibody production
Too much uric acid may cause gout attacks.
• Joint pain caused by gout. Gout may happen as a result of excessive uric acid production.
• Portal hypertension is caused by a progressively enlarging spleen. Portal hypertension can lead to varices within the stomach and esophagus, which may rupture and bleed. Liver function may be compromised as well.
• Abnormal growth of blood-forming cells outside of the bone marrow (called extramedullary hematopoiesis) can occur in different parts of the body, including lymph nodes, lungs, and spinal cord, causing symptoms in these areas.
• Cutaneous myelofibrosis is a rare skin disease characterized by skin and subcutaneous nodules.
Physically:
- Splenomegaly is present and sometimes massive (cardinal feature).
The continued enlargement of the spleen may lead to increased satiety and painful attacks of splenic infarction may occur.
- Hepatomegaly is present in 50% of cases.
- Later progressive bone marrow failure takes place as the marrow becomes fibrotic.
- Anemia-----severe where the RBC transfusion necessary
- Thrombocytopenia bleeding
- Later in course of the disease; the patient becomes cachectic and may experience severe bone pain especially lower legs.
- Hematopoiesis in the liver, portal hypertension, ascites, esophageal varices, liver failure.
How is Myelofibrosis diagnosed?
Primary myelofibrosis is diagnosed by combining physical examination (showing enlarged spleen), blood test, and bone marrow examination.
Only after excluding other causes of myelofibrosis (including leukemia, lymphoma, and other types of cancer that have spread to the bone marrow), is the diagnosis of primary myelofibrosis.
Laboratory finding:
1. CBC(complete blood count) with blood smear:
Anemia is usually present and usually increases over time. RBCs are poikilocytic.
There may be reticulocytosis and polychromatophilia, teardrop-shaped red blood cells (dacryocytes) are a typical morphological feature.
Nucleated red blood cells and neutrophil precursors are usually present in peripheral blood. The white blood cell count usually increases, but it varies greatly.
A low white blood cell count often indicates a poor prognosis. Neutrophils are regularly immature, and myeloblasts may be present, even in the absence of acute leukemia.
The initial platelet count may be high, normal, or decreased; however, as the disease progresses, thrombocytopenia tends to replace it.
In the early stages of this disease, the number of white blood cells and platelets may be found to be higher than normal, but low white blood cell and platelet numbers are common in more advanced diseases.
The triad of TEARDROP POIKILOCTOSIS, LEUKOERYTHROBLASTIC, GAINT ABNORMAL PLATELETS is almost diagnostic of myelofibrosis.
2. Bone marrow examination
- cannot be aspirated (dry tap), biopsy is preferred.
- Though early in the course of the disease, it is hypercellular with a marked increase in megakaryocyte.
- At this stage, fibrosis is detected by silver staining, indicating an increase in reticulin fibers.
- Because it is necessary to prove myelofibrosis and fibrosis may be unevenly distributed, if the first biopsy cannot be diagnosed, the biopsy should be repeated at different sites.
3. Genetic testing
About 50% of patients have a JAK2 mutation. Some have a mutation of the calreticulin gene.
Differential diagnosis:
• Metastatic carcinoma
• Hodgkin’s disease
• Hairy cell leukemia
• Tuberculosis
• Polycythemia rubra vera
• Essential thrombocytopenia
• CML
• Exposure to benzene
Treatment:
- In the past, the treatment of myelofibrosis was based on the symptoms and degree of low blood cells.
- In young people, bone marrow or stem cell transplantation seems to improve the appearance and cure the disease.
A long-term (5 years) remission is possible for some patients with bone marrow transplantation. Younger patients and some other patients should consider this treatment.
- There is no specific treatment: Because myelofibrosis usually progresses slowly, people with myelofibrosis may survive for 10 years or more, but the result depends on bone marrow function.
Occasionally, the disorder worsens rapidly. Treatment aims to delay the progression of the disease and reduce complications.
A known treatment method is allogeneic stem cell transplantation, but this method has major risks. Other treatment options are largely supportive and do not alter the course of the disorder (with the possible exception of ruxolitinib).
These choices may include regular folic acid, aloopurinol, or blood transfusion.
Dexamethasone, interferon-alpha, and hydroxyurea (also called hydroxyurea) may work.
- Anemic patients ------RBC transfusion
- Androgens Oxymetholone or Testosterone
- Lenalidomide and thalidomide can be used for treatment, although peripheral neuropathy is a common troublesome side effect.
- Recombinant erythropoietin (epoetin alfa) helpful in a small number of patients to stimulate the bone marrow for red blood cell synthesis.
- Splenectomy (routinely not performed) except in:
- Severe thrombocytopenia
- High RBC transfusion requirement
- Recurrent painful episodes with a huge spleen.
- Massive splenomegaly
Prognosis depends on the following:
- The age of the patient.
- The number of abnormal red and white blood cells.
- The number of blasts in the blood.
- Whether there are any changes in chromosomes.
- Whether the patients have symptoms such as fever, night sweats, or weight loss.





Comments
Post a Comment