Anemia of chronic disease (ACD)
Definition:
- Anemia of chronic disease is a type of anemia that occurs in patients with infectious, inflammatory, or neoplastic diseases that stay for more than 1 or 2 months.
- It does not involve anemias caused by marrow replacement, blood loss, hemolysis, renal insufficiency, hepatic disease, or endocrinopathy, even when these disorders are chronic.
Epidemiology
The ACD is extremely common
- Anemia of chronic disease is more frequent than any anemia syndrome other than blood loss with consequent iron deficiency.
- Anemia of chronic disease is the most common cause of anemia in inpatients.
- After excluding patients with bleeding, hemolysis, or known hematological malignancies, 52% of anemia patients met the laboratory standards for anemia of chronic diseases.
- Anemia of chronic disease was observed in 27% of outpatients with rheumatoid arthritis, and 58% of chronic disease was observed in newly admitted patients in the rheumatology department of the hospital.
Disorders Related with the Anemia of Chronic Disease ACD:
● Chronic infections
- Pulmonary infections: abscesses, emphysema, tuberculosis, pneumonia.
- Subacute bacterial endocarditis
- Pelvic inflammatory disease
- Chronic urinary tract infections
- Chronic fungal disease
- HIV infections
- Osteomyelitis
● Chronic, noninfectious inflammations
- Rheumatoid arthritis
- LES (Systemic lupus erythematosus)
- Severe trauma, thermal injury
- Vasculitis
● Malignant diseases:
- Cancer
- Hodgkin’s disease and Non-Hodgkin’s Lymphomas
- Leukemias
- Multiple myeloma
● Miscellaneous:
- Alcoholic liver disease
- Thrombophlebitis
- Ischemic heart disease
● Idiopathic ACD
Pathogenesis
● Shortened red cell life span, moderately 20-30% (from 120 to 60-90 days)
● Relative bone marrow(erythropoiesis) failure:
- Cytokines liberated by inflammatory cells (TNF-α, IL-1, IFN-γ) affect erythropoiesis by inhibiting the growth of erythroid progenitor cells.
- Compared with healthy subjects, the serum erythropoietin level of patients with anemia of chronic disease is normal but much lower than that of patients with non-ACD anemia.
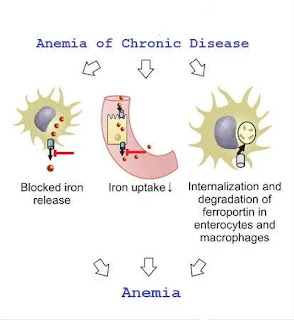
● Abnormal Iron Metabolism
- Activation of the reticuloendothelial system with increased iron retention and storage inside it.
- The release of iron from macrophages to circulating transferrin is blocked (Iron reuse is impaired).
- Reduced concentration of transferrin
(reduced production, increase sequestration in the spleen and the foci of inflammation, increase loss ).
Symptoms:
- Symptoms of the primary disease ( malignancy or chronic inflammatory disease)
- Symptoms of the anemia
laboratory features:
● The anemia is most often mild or moderate ( Hb 7-11g/dl).
- lower values are observed in 20-30% of patients.
● The anemia is usually normochromic and normocytic (MCHC and MCV are normal)
- MCV 70-80 fl in 5-40% of Anemia of chronic disease patients.
- MCHC 26-32 g/dl in 40-70%
● Erythrocyte sedimentation rate (ESR) - usually rapid.
● Reticulocytes - Usually normal or slightly decreased number, rarely increased number.
● Iron metabolism
1. Serum iron-reduced (necessary for the diagnosis of ACD).
2. TIBC - reduced or low-normal.
3. Transferrin saturation(TS) - moderately reduced
( over than in iron-deficiency anemia), usually > 10%.
4. Serum Ferritin-increased or normal.
5. Serum Transferrin Receptor (sTR)-Normal.
6. Sideroblasts in the bone marrow-reduced (5-20%).
Differential diagnosis:
|
Laboratory features |
Iron deficiency
|
ACD |
|
|
|
without iron deficiency |
with iron deficiency |
|
|
Serum Fe |
Decreased |
Decreased |
Decreased |
|
TS |
Decreased <10% |
Decreased >10% |
Decreased <10% |
|
TIBC |
Increased |
Decreased, N |
N, Decreased |
|
sFerritin |
Decreased <10mg/L |
Increased >200mg/L,N |
Decreased <30mg/L,N |
|
Sideroblasts |
<10% |
10-20% |
<10% |
|
sTR |
Increased |
N |
Increased |
Advantages of ACD for patients(?!)
- Withdrawal of iron by increased storage of the metal within the reticuloendothelial system acts to limit the availability of iron to microorganisms or tumor cells and thereby inhibit their growth and proliferation.
- Decreased hemoglobin reduces the oxygen transport capacity of the blood and decreases the overall oxygen supply, which may primarily affect rapid proliferating (malignant) tissues and micro-organism
- Retention and storage of iron in the reticuloendothelial system directly and indirectly via cytokines strongly affect cell-mediated immune function.
Therapy:
1. Treatment of the underlying disorder.
2. Iron supplementation (IS):
- for patients with ACD with chronic infection or malignancy IS should be strictly avoided.
- IS benefits patients with ACD associated with auto-immune or rheumatic disorders.
- when ACD is complicated by iron deficiency (about 27% patients.)
Anemia of chronic disease (ACD) -therapy (2)
3. Transfusion demand (about 30% )patients who have low Hb and are symptomatic.
4. Recombinant erythropoietin 10.000 units 3 times a week I .v. or s.c. If there is still no response, the treatment should be discontinued. (in 40% of patients it reduces the number of transfusions).
5. Sequential administration of erythropoietin and iron(48h later).
5. Iron chelation with deferoxamine - in some patients therapy was associated with a rise in hemoglobin level.
6. In future anti-TNF-antibodies.


Comments
Post a Comment