Case study (42) - HIV-positive patient with infection with Pneumocystis carinii.
A 34-year-old patient, with a history of intravenous drug abuse, presents with a 7-day history of progressive shortness of breath.
On examination, he is pyrexia and has clear dyspnea and tachycardia.
His blood pressure is reduced to 90/60 mmHg. Oxygen saturation when breathing 40% oxygen is reduced at 86%, and he is sweating.
Full blood count shows:
Hemoglobin (Hb) 85 g/L
White blood cells (WBC) 17.5 X 109/L (neutrophils 79%)
Platelets 105 X 109
Questions:
Q1. What is the likeliest diagnosis from the history and chest x-ray?
Q2. What further tests should be performed?
Q3. How should he be treated?
Q4. What other hematological complications will occur in this situation?
Answers:
A1. He probably has an infection with Pneumocystis carinii.
A2. HIV antibody. Bronchoalveolar lavage or bronchial secretions should be obtained so that a firm microbiological diagnosis can be made; this should be done after consultation with an anesthetist.
He needs to be checked out for admission to an intensive therapy unit.
A comprehensive biochemical screen should be performed, and blood, urine, and throat swabs should be sent for bacteria, viruses, fungi, and protozoa culture.
A3. He should be treated with high-dose intravenous co-trimoxazole for presumed Pneumocystis infection, but broad-spectrum antibiotics should be given until a bacteriological diagnosis is proven and in case of mixed infections.
Large doses of co - trimethoprim may cause bone marrow suppression, which can be partially reversed with folinic acid.
A4. Immune thrombocytopenia, lymphopenia, and anemia of chronic disease are relatively common.
The commonest hematological malignancy associated with HIV is non-Hodgkin’s lymphoma; high-grade Burkitt-like B-cell lymphoma with central nervous system (CNS) involvement is characteristic (see Figure below).
Paraproteins and myeloma may occur, and acute myeloid leukemia (AML) is reported. Monocytosis, hemophagocytic syndrome, immune hemolytic anemia, myelodysplasia, and aplastic anemia are also reported.
The blood film below is from an HIV-positive patient who is on zidovudine; it shows macrocytosis and thrombocytopenia.
The Figure below shows bone marrow aspirate from the same patient – he has developed acute myeloid leukemia with erythroid differentiation.
Myelodysplasia and acute leukemia are reported.
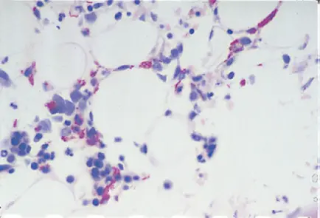
A Ziehl–Nielson staining on a bone marrow trephine biopsy in an HIV-positive patient, the figure below shows A variety of organisms were identified as intracellular Mycobacterium avium - intracellulare when cultured.
Bone marrow trephine biopsy in an HIV-positive patient, the Figure below shows infection with Cryptococcus neoformans.







Comments
Post a Comment