CHRONIC MYELOPROLIFERATIVE NEOPLASMS (MPN)- Essential Thrombocythemia (ET)
Essential thrombocythemia (ET), together with polycythemia vera (PV) and primary myelofibrosis (PMF), is a clonal Ph-negative myeloproliferative neoplasm (Ph- MPN), characterized by thrombocytosis, bone marrow megakaryocytic hyperplasia, and a tendency to develop vascular complications.
ET is slightly more frequent in males than in females. Can occur at any age, but rarely occurs in children.
Etiology
- Autonomous production
• CFU-Meg form colonies in the absence of exogenous thrombopoietin (Tpo.)
- Increased sensitivities to Cytokines (interleukin-3 [IL-3]).
- The effect of platelet inhibitory factor (transforming growth factor [TGF] β) is reduced.
Mutation
1. Janus kinase 2 (JAK2) V617F
• 50% in ET patient
• Permanently turn on thrombopoietin receptors, leading to overproduction of megakaryocytes.
2. Calreticulin (CALR)
• 25% of ET patient
• Exclusive of JAK 2 and MPL mutation
3. Myeloproliferative leukemia virus oncogene (MPL)
• 3-5% of ET patient
• constitutive activation of the thrombopoietin receptor protein.
Clinical presentation
- 25-33% of patients asymptomatic at diagnosis.
- Hemorrhage and thrombosis
• Reduce the aggregation of various chemical substances, excessive aggregation, and intracellular concentration.
• Decrease in von Willebrand ristocetin cofactor activity. (platelet count >1mil).
• Protein C, and protein S, and Acquired antithrombin III, deficiency.
- Hemorrhagic tendency
• Easy bruising
• The gastrointestinal tract is the main site of bleeding complications.
• Other bleeding sites include skin, eyes, gums, urinary tract, joints, and brain.
• Bleeding is usually not serious and blood transfusions are rarely needed.
• Bleeding is usually related to platelet counts greater than 1 million/μL.
- Thrombotic tendency
• Erythromelalgia
• Ocular migraine
• TIA
• Occlusion of the legs, coronary and renal arteries.
• Venous thrombosis of the spleen, liver, or leg and pelvic veins may occur.
• Pulmonary hypertension may result from pulmonary vasculature occlusion.
- On Examination: 40-50% present with splenomegaly and 20% present with hepatomegaly.
Laboratory investigations
1. Complete blood count: sustained, unexplained elevation in the platelet count and mild neutrophilic leukocytosis.
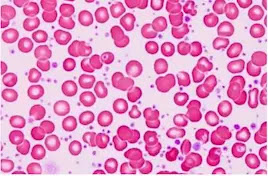
2. Peripheral smear: Increased platelet number and large and hypogranular and clumps platelets.
3. Coagulation profile: PT and aPTT normal
4. Bleeding time: Maybe prolonged
5. Serum potassium: Hyperkalemia (lab artifact not demonstrated by ECG.)
6. Platelet aggregation studies: impaired platelet aggregation. Spontaneous platelets aggregation.
7. Bone marrow biopsy: Hypercellular marrow (90%) with Megakaryocytic hyperplasia and Giant megakaryocyte with staghorn and hyperlobulated nuclei.
Even if other studies do not support iron deficiency (bleeding), bone marrow iron staining results may be negative.
8. Genetic studies: JAK2 V617F, CALR, and MPL mutations.
Diagnosis WHO 2008
|
Essential Thrombocythemia |
Major criteria |
Minor criteria |
|
Platelet count ≥ 450x109/L |
|
|
|
Bone marrow biopsy showing megakaryocyte
proliferation with increased numbers of enlarged, mature megakaryocytes, no or little
granulocyte or erythroid proliferation, and very rarely minor (grade 1)
increase in reticulin fibers. |
√ |
|
|
Not meeting WHO criteria for PV, primary
myelofibrosis, BCR-ABL positive CML, MDS, or other myeloid neoplasms. |
√ |
|
|
Demonstration of JAK2, CA, or MPL mutation. |
√ |
|
|
Presence
of a clonal marker or absence of evidence for
reactive thrombocytosis. |
|
√ |
Diagnosis requires meeting all 4 major criteria or the first 3 major criteria and the minor criteria.
Differential diagnosis:
1. Chronic myeloid leukemia (CML)
• Ph chromosome analysis
• Fluorescence in situ hybridization (FISH) for bcr-abl.
2. Polycythemia vera (PV)
• Red cell mass and plasma volume determination.
3. Primary myelofibrosis (PMF)
4. Secondary thrombocytosis
• Elevation of C-reactive protein (CRP), fibrinogen, and interleukin 6 levels (acute phase reactant)
Treatment
The high-risk factor for thrombohemorrhagic event:
• Age >60 years
• History of thrombosis
• Platelets count more than 1500 x 10 9/L (1.5 million/μL).
• Obesity
• Cardiovascular RF (smoking, hypertension, and hypercholesterolemia)
• Hypercoagulability markers (Factor V Leiden, antiphospholipid antibody)
• JAK2 mutation
• Lifestyle modifications should be recommended
• Cytoreductive therapy to decrease the platelet count
– Hydroxyurea
– Low dose aspirin
– Busulfan
– Anagrelide
– Interferon alfa
– Phosphorus-32 (32 P)
Low-risk patient
• Observation may be appropriate
• Low-dose aspirin may be helpful for patients with symptoms of microvascular occlusion (erythromelalgia).
Plateletpheresis
• In emergency temporary inefficient remedy
• acute thrombosis and/or marked thrombocytosis
Surgery
• increased risk for bleeding and thrombosis
• Cytoreductive therapy
Prognosis
• Life expectancy is almost the life expectancy of healthy people.
• A retrospective study revealed:
– 5-year survival rate of 81%
– 10-year survival rate of 64%



Comments
Post a Comment