Hematopoiesis: the process of the formation and development of blood cells
Hematopoiesis is the process of the formation and development of blood cells.
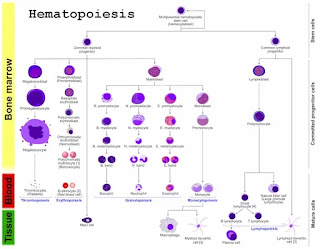
Hematopoiesis in humans occurs in bone marrow exclusively. All cellular elements derived from pluripotent stem cell (PPSC)PPS retains the ability to both replicate itself and differentiate Types of differentiation determined by the influence of various cytokines, only mature cells are released into the peripheral blood.
Hematopoiesis is the process of the formation and development of blood cells. Hematopoiesis in humans occurs in bone marrow exclusively. All cellular elements derived from pluripotent stem cell (PPSC)PPS retains the ability to both replicate itself and differentiate Types of differentiation determined by the influence of various cytokines, only mature cells are released into the peripheral blood.
Hematopoiesis in humans occurs in bone marrow exclusively.
Why do we need Hematopoiesis?
blood Cells are constantly being lost or destroyed. Thus, to maintain the formation and development of blood cells, the system must have the capacity for self-renewal.Sites of production of blood cells:
- Fetus: 0-2 months (yolk sac).
- 2-7 months (liver and spleen)
- 5-9 months (bone marrow).
- Infants: bone marrow
- Adults: bone marrow, ribs, sternum, skull, sacrum, and pelvis.
Hematopoiesis inside the bone marrow is named medullary Hematopoiesis.
Hematopoiesis in areas other than the bone marrow is called extramedullary Hematopoiesis Extramedullary Hematopoiesis may occur in fetal hematopoietic tissue (liver and spleen), and an adult when the bone marrow cannot meet the physiologic needs of the tissues.
This can lead to hepatomegaly and/or splenomegaly (increase in the size of the liver or spleen because of increased functions in the organs).
Erythropoiesis:
Erythropoiesis, the process of making erythrocytes begins with the formation of proerythroblasts from hemopoietic stem cells.From three to five days, several stages of development follow as ribosomes proliferate and hemoglobin is synthesized.
Finally, the nucleus is ejected, producing depression in the center of the cell. Young erythrocytes, called reticulocytes, still containing some ribosomes and endoplasmic reticulum, pass into the bloodstream, and develop into mature erythrocytes after another one or two days.
Erythropoietin:
Erythropoietin (EPO), a hormone produced mostly by the kidneys, stimulates the bone marrow to produce erythrocytes.When inadequate amounts of oxygen are delivered to body cells, a condition called hypoxia, the kidneys increase EPO secretion, which, in turn, stimulates an increase in erythrocyte production.
The production rate of erythrocytes in healthy individuals is two million cells per second.
Normal production requires adequate amounts of iron and vitamin B12 and folic acid.
Leukopoiesis:
Leukopoiesis, the process of making leukocytes, is stimulated by various colony-stimulating factors(CSFs), hormones produced by mature white blood cells. The development of each kind of white blood cell begins with the division of hemopoietic stem cells into one of the following “blast” cells.
• Myeoblasts develop to form eosinophilic, neutrophilic, or basophilic myelocytes, which lead to the development of the three kinds of granulocytes.
• Monoblasts lead to the development of monocytes.
• Lymphoblasts lead to the development of lymphocytes.
Thrombopoiesis:
Thrombopoiesis, is formation of platelets, begins with the formation of megakaryoblasts from hemopoietic stem cells.The megakaryoblasts develop without cytokinesis to become megakaryocytes, huge cells with a large, multilobed nucleus. The megakaryocytes then fragment into segments as the plasma membrane enfolds into the cytoplasm.
Hemopoietic Cells:
The basis of Hematopoiesis is a small population of self-replicating stem cells, which ultimately can generate all types of blood cells.Their progeny may develop into either lymphocytic stem cells or pluripotent stem cells (colony-forming unit - stem cell - CFU-S).
The pluripotent stem cells gives rise to stem cells which can form the major groups of blood cells other than lymphocytes.
Depending on their progeny it is possible to differentiate
• burst-forming unit of the erythroid line (BFU-E),• colony-forming unit - granulocytes, and macrophages (CFU-G/M), and
• colony-forming unit - megakaryocytes (CFU-Mk).
Erythrocytes:
• The first stage of erythropoiesis is the proerythroblast - a large, slightly basophiliccell, which contains a large, lightly stained nucleus.
• Proerythroblasts proliferate to generate a sequence of cells that show a gradual decrease in size and condensation of their chromatin.
• They are called after changes in the staining characteristic of their cytoplasm (basophilic
erythroblast, polychromatophilic and orthochromatic normoblasts).
• The nucleus is later extruded from the normoblast.
• The cell enters the circulation as a reticulocyte, which still contains some organelles.
• Reticulocytes Saty for a few days in the bone marrow or the spleen to mature to erythrocytes.
• In some blood smears reticulocytes may be recognizable because of a very slight basophilic
staining - either homogeneous or in the form of a basophilic stippling.
Granulocytes:
• Myeloblast appears light-microscopically like proerythroblast.• They proliferate to generate promyelocytes. Promyelocytes begin to gather nonspecific granules, but they are still able to divide.
• The maturation of their progeny, the myelocytes, is characterized by the accumulation of specific granules and changes in nuclear morphology. Metamyelocytes have a C-shaped nucleus.
Blood Platelets (Thrombocytes):
• are, as mentioned above, fragments of the cytoplasm of megakaryocytes.• Megakaryocytes are large cells (up to 160 μm in diameter), which contain very large, highly lobulated, polyploid nuclei.
• Megakaryocytes are the product of the differentiation of basophilic megakaryoblasts.
All the various types of blood cells:
• are produced in the bone marrow.• Originate from a single type of cell called a hematopoietic stem cell — an "adult" multipotent stem cell.
These stem cells
• Are a few (only about one in 10,000 bone marrow cells).• Are attached (probably by adherents’ junctions) to osteoblasts lining the inner the surface of bone cavities.
• Express a cell‐surface protein designated CD34.
• Produce, by mitosis, two kinds of progeny:
- more stem cells (self-renewal).
- cells that begin to differentiate along the paths leading to the various kinds of blood cells.
Which way is taken is regulated by the need for more of that type of blood cell which is, in turn, controlled by appropriate cytokines and/or hormones.
For example, Interleukin-7 (IL-7) is the major cytokine in stimulating bone marrow stem cells to start down the
"lymphoid" path leading to the various lymphocytes (mostly B cells and T cells).
Some of the cytokines that drive the differentiation of the "myeloid" leukocytes are:
1. Erythropoietin (EPO), produced by the kidneys, enhances the production of red blood cells (RBCs).2. Thrombopoietin (TPO), assisted by Interleukin‐11 (IL‐11), stimulates the production of megakaryocytes. Their fragmentation produces platelets.
3. Granulocyte‐macrophage colony‐stimulating factor (GM‐CSF), as its name suggests, sends cells down the path leading to both those cell types. Opportunely, one path or the other is taken.
- Under the influence of granulocyte colony‐stimulating factor (G‐CSF), they differentiate into neutrophils.
- Further stimulated by interleukin‐5 (IL‐5) they develop into eosinophils.
- Interleukin‐3 (IL‐3) participates in the differentiation of most of the white blood cells but plays a particularly prominent role in the formation of basophils
- Stimulated by macrophage colony‐stimulating factor (M‐CSF) the granulocyte/macrophage progenitor cells differentiate into monocytes, macrophages, and dendritic cells (DCs).
HEMATOPOIETIC FACTORS
|
NAME |
CELLULAR
SOURCE |
CELL
TYPES PRODUCED |
|
Erythropoietin
(EPO) |
Kidney
cells, Kupffer cells |
red
blood cells |
|
G-
colony-stimulating factor |
Monocytes,
fibroblasts, endothelial cells |
neutrophils |
|
M-
colony-stimulating factor |
Monocytes,
fibroblasts, endothelial cells |
monocytes |
|
GM-
colony-stimulating factor |
T
cells, monocytes, fibroblasts,
endothelial cells |
neutrophils,
monocytes, eosinophils, basophils, megakaryocytes, red blood cells |
|
Interleukin
-1 |
Macrophages,
endothelial cells,
fibroblasts |
neutrophils,
monocytes, eosinophils, basophils, megakaryocytes, red blood cells |
|
Interleukin
-3 |
T
cells |
neutrophils,
monocytes, eosinophils, basophils, megakaryocytes, red blood cells |
|
Interleukin
-4 |
T
cells |
basophils |
|
Interleukin
-5 |
T
cells |
eosinophils |
|
Interleukin
-6 |
Macrophages,
endothelial cells,
fibroblasts |
neutrophils,
monocytes, eosinophils, basophils, megakaryocytes, red blood cells |





Comments
Post a Comment