Case study (35) - Autoimmune hemolytic anemia.
A 6-year-old girl has a 4-week history of increasing fatigue and lack of energy.
She has also become jaundiced.
There is no relevant past medical history.
The examination revealed that the pale, jaundiced child had no lymphadenopathy, but the spleen was palpable 6 cm below the left costal margin.
There are no signs of chronic liver disease.
Cardiovascular examination reveals a soft apical systolic murmur.
Laboratory Investigations:
Hemoglobin (Hb) 61 g/L
Mean corpuscular volume (MCV) 110 fL
Reticulocytes 22%
White blood cells (WBC) 15.1 X 109/L
Questions:
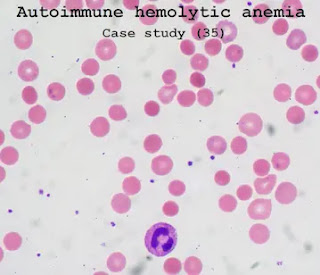
Q1. What abnormalities are seen in the blood film?
Q2. What is the likely diagnosis?
Q3. What further investigations are indicated?
Q4. How would you treat this patient?
Answers:
A1. The blood film shows polychromasia, anisocytosis, poikilocytosis, and spherocytes, with circulating nucleated red blood cells.
A2. Autoimmune hemolytic anemia.
A3. Direct antiglobulin test (DAT, Combs test) is strongly positive, complement and IgG can be detected on the surface of red blood cells.
Liver function tests show elevated bilirubin (320 mmol/L) which is mostly unconjugated.
Her serum contains pan-reactive red blood cell antibodies
There is no clear specificity and no evidence of other red blood cell alloantibodies.
The antibody reacts most strongly at 37°C.
Serum haptoglobin is often reduced and urine hemosiderin is present in the presence of intravascular hemolysis.
Autoantibody screening showed a positive antinuclear factor (ANF) when the titer was> 1:100, indicating potential systemic lupus erythematosus (SLE).
A computed tomography (CT) scan of the abdomen showed an enlarged spleen, but no enlarged lymph nodes and no evidence of underlying lymphoma.
Red blood cell grouping and blood selection for cross-matching should be carefully performed in an experienced laboratory.
Important infectious causes of autoimmune hemolytic anemia (AIHA) in children include Epstein–Barr virus (EBV), cytomegalovirus (CMV), mycoplasma, and parvovirus.
A4. Prednisolone 1.0 mg/kg of body weight is first-line immunosuppression.
Azathioprine, cyclophosphamide, and cyclosporine can be considered, but if possible, they should be avoided in children.
The anti-CD20 monoclonal antibody rituximab may be considered. Folic acid 5 mg should be given daily.
Splenectomy will reduce the destruction of red blood cells and eliminate the production of autoantibodies.
However, the risk of infection increases
After surgery, it is best to avoid surgery for children under 5 years of age.
Before splenectomy, pneumococcal and Hemophilus influenzae type b vaccine must be inoculated, and then long-term prophylactic penicillin treatment.
Evans syndrome is an association between AIHA and immune thrombocytopenic purpura (ITP), and it is seen in more than one-third of AIHA children.


Comments
Post a Comment