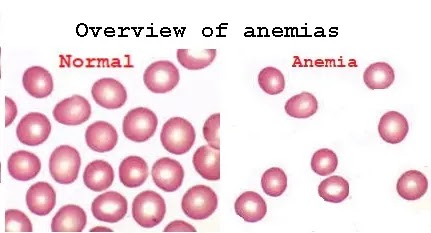
Overview of anemias
Definition of Anemia
Anemia is a reduction in the RBC count, Hb, and/or HCT values while compared to the normal reference value for age and sex.
True anemia:
- Decreased RBC mass and normal plasma volume.
Pseudo or dilutional anemia:
- Normal RBC mass and increased plasma volume.
An increase in plasma volume can occur in Pregnancy, volume overload (IVs), and congestive heart failure.
In general, anemia is not a disease, but it is the expression of an underlying disorder or disease.
The diagnostic criteria for anemia are decrease Hb, Hct, or RBC.
Pathophysiology
A decrease in RBCs, Hb, or Hct level Lead to Diminished O2-Carrying capacity Lead to Hypoxia and hypoxia-induced effects on organ function Appeared Signs and symptoms of anemia.
When RBC loss or destruction exceeds the maximal capacity of bone marrow RBCs production or when bone marrow production is impaired. (Increase destruction or decrease production).
Hematologic Response to Anemia
- Tissue hypoxia leads to an increase in the renal release of erythropoietin (EPO) to stimulate bone marrow erythropoiesis.
- The normal bone marrow can increase its activity 5-10 times normal Marrow becomes hypercellular
Signs of Accelerated Bone Marrow Erythropoiesis
1- Hypercellular BM: erythroid hyperplasia.
2- Nucleated RBCs
3- Reticulocytosis
If the demand exceeds maximal bone marrow activity, RBC production may take place in extramedullary sites, liver, spleen (hepatosplenomegaly).
Reticulocyte
Reticulocyte = non-nucleated RBC contains polyribosomal RNA as stained by supravital stain (new methylene blue or brilliant cresyl blue).
Reticulocyte percentage (%): manual counting of Retics in 1000 RBCs in the stained smear (25 in 1000 RBCs, so Retics 2.5%).
General Symptoms and Signs of Anemia
The signs and symptoms can be connected to the anemia itself, or the underlying cause.
- Weakness & Fatigue
- Dizziness
- Shortness of breath
- Confusion, poor concentration.
- pale skin, pale mucosal linings, and pale nail beds).
In very severe anemia
- Palpitations
- Angina (if preexisting heart disease is present)
- Heart failure (Hb 5).
- Flow murmurs.
Specific symptoms and signs exhibited may include:
Koilonychia (spoon-shaped nails are seen in iron deficiency anemia (IDA).
Jaundice when anemia results from an abnormal break down red blood cells in hemolytic anemia),
Bone deformities (found in thalassemia major)
Leg ulcers: (seen in sickle cell disease)
Organomegaly.
Significance of anemia and compensatory mechanisms
The signs and symptoms of anemia extend from slight fatigue to life-threatening reactions depending upon
- Onset
- Severity
- The ability of the body to adapt
In summary, anemia may develop:
● When RBC loss or destruction exceeds the maximal capacity of bone marrow RBC production.
● When bone marrow production is impaired.
Classification of Anemia
1- Based on morphology (the Size, and Hb content of RBCs):
a. Microcytic anemia:
- Iron deficiency anemia.
- Thalassemia.
- Sideroblastic anemia.
- Anemia of chronic disease (Severe Cases).
- Lead poisoning.
b. Normocytic normochromic anemia:
- Hemolytic anemia.
- Anemia of chronic disease (most cases).
- Chronic kidney disease.
- Iron deficiency anemia (early).
- Combined nutritional deficiencies (iron & folate or cobalamin)
- A plastic anemia.
c. Macrocytic anemia:
- Megaloblastic anemia.
- Liver disease.
- Hypothyroidism.
- Myelodysplasia.
- Reticulocytosis.
2. Classification Based on Pathophysiology (Cause)
a. Hemorrhage / Hemolysis:
- Blood loss.
- Intravascular Hemolysis.
- Autoimmune disease.
- Hemoglobinopathy.
- Metabolic/membrane defect.
b. Increased red cell destruction.
- Extravascular hemolytic disease: (autoimmune disorders, infection (e.g. malaria), hypersplenism, trauma to red blood cells).
- Intravascular hemolytic disease (hereditary membrane or globin synthesis abnormalities).
c. Decreased red cell production.
- Nutritional deficiencies: (iron, B12, or folate)
- Decreased number of erythroblasts (as in aplastic
anemia).
- Bone marrow infiltration by malignancy.
- Sideroblastic anemia
- Anemia of chronic disease
Diagnosis of anemia
To make a clinical diagnosis of anemia.
A. Patient history
B. Physical exam
C. Lab investigations
Work- up for diagnosis of anemia
● Be sure it is a case of anemia:
(Symptoms, Signs, blood picture)
● Identify the type of anemia:
(Microcytic, macrocytic, or normocytic)
● Identify the cause
- Iron, folate, or B12 deficiency.
- Secondary causes: colon cancer, stomach surgery.
● M: Hb <N Hct <N
F: Hb <N Hct <N
Then
[check MCV]
Then
▪If MCV <80 = microcytic
- Fe deficiency (through Iron studies)
- Thalassemia (Through Hb-Electrophoresis)
▪If MCV >95 = macrocytic
- megaloblastic anemia
- Non megaloblastic:
▪If MCV 80-95 = normocytic
Then
[check reticulocyte count]
- Low reticulocyte:
▪Normocellular/Hypercellular Bone Marrow: MAY BE Anemia of malignancy.
▪Acellular BM: Aplastic anemia
- High reticulocyte:
1. Look for evidence of hemolytic anemia.
2. Tonics (a vitamin supplement)
3. Hemorrhage.



Comments
Post a Comment